RE Official Information Act request WCDHB 9353
I refer to your email dated 3 October 2019 requesting the following information under the Official Information Act from West Coast DHB regarding West Coast patient movements. I note your request was clarified on 4 October 2019 as below:
1. In the 2018/2019 year to June, how many patients were sent back to their GP after their first specialist appointment?
Having attended and been seen at their First Specialist Appointment (FSA) with a Specialist at West Coast DHB publicly funded medical and surgical outpatient clinics during 2018-19, a total of 1,429 patients had the outcome for their presenting referral completed with no further need for ongoing specialist care or other treatment, and were appropriately discharged and returned back to their general practice as a result.
Only one patient was referred back to their general practitioner because they were below threshold for service following their FSA.
There were no patients where it was decided that treatment was not the best option however, one patient who was seen, declined further treatment for follow-up at their own request.
Outcomes for the remainder of patients seen at their FSA were either acceptance onto the waiting list, arranged admission, and referral for further additional investigative and follow-up services.
In all, 4,462 people attended and were seen at their First Specialist Appointment with a Specialist at West Coast DHB medical, surgical or first appointment minor operations outpatient clinics during 2018-19 as measured through National Patient Flow.
2. How many patients were sent to ChCh for orthopaedic surgery in the year to June (2018/2019)?
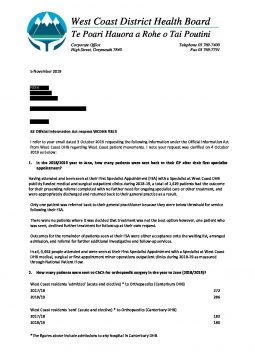
West Coast residents ‘admitted’ (acute and elective) * to Orthopaedics (Canterbury DHB)
2017/18 272
2018/19 286
West Coast residents ‘sent’ (acute and elective) * to Orthopaedics (Canterbury DHB)
2017/18 182
2018/19 180
*The figures above include admissions to any hospital in Canterbury DHB.
The figures for ‘sent’ to orthopaedics include elective admissions and acute patients transferred from the West Coast. The difference between those figures and the total admissions is due to West Coast residents already in the Canterbury region.
3. How many orthopaedic surgery procedures were done in Greymouth in the year to June (2018/2019)?
• How many orthopaedic surgeons are on the roster?
During the 2018/19 financial year, there have been 487 orthopaedic public (non-ACC) patients discharged from Grey Base Hospital, including 242 acute patients and 245 elective (arranged and waiting list) patients. Of these, 80 acute patients and 186 elective cases had operation procedures undertaken.
During this period there were five orthopaedic surgeons on the roster, and increasing to six on the roster from the start of May 2019.
4. How many patients had elective surgery in Greymouth in the year to June (2018/2019)?
A total of 1,558 elective surgery procedures (all types) were conducted in the operating theatres at Grey Base Hospital in the financial year to 30 June 2019.
5. How many patients from the Coast were admitted to ChCh hospital and-or had surgery in ChCh in the year to June (2018/2019)?
West Coast residents admitted (acute and elective) to Canterbury DHB/Facilities
2017/18 1806
2018/19 1919
West Coast residents admitted (acute and elective) to Christchurch Hospital
2017/18 1474
2018/19 1562